by Dr. Stefanie Morlok, München, Utting am Ammersee und St. Gallen
TMJ Disorders After a Car Accident – When the Jaw is Affected
Temporomandibular joint disorders (TMJ or TMD) are often known for causing jaw pain, muscle tension, or teeth grinding. What’s less well known is that even a car accident – without visible injuries – can trigger or worsen TMJ dysfunction, particularly when there is a preexisting malocclusion such as a deep bite.
In this article, you’ll learn:
-
How a car accident can affect the jaw
-
What symptoms to watch out for
-
What you can do to recover and feel better
-
What scientific studies say about the connection
What Happens to the Jaw in a Car Accident?
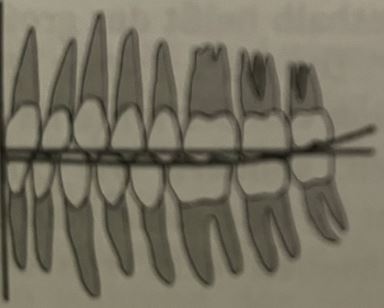
In a rear-end collision or whiplash injury, most people think of the neck first. But the temporomandibular joint (TMJ) can also be significantly affected by the sudden movement or instinctive jaw clenching during the impact.
Studies have shown that patients with certain occlusal conditions – such as deep overbite or retrodisplaced condyles – are particularly vulnerable, as the biomechanical forces during trauma are more likely to destabilize the jaw joint [1][2].
Common effects on the jaw joint include:
-
Compression or overstretching of the TMJ
-
Misalignment of the jaw position
-
Overload of the masticatory (chewing) muscles
-
Development or worsening of TMJ dysfunction
Signs of TMJ Dysfunction After an Accident
Symptoms may appear weeks or even months after the accident – making it harder to link them to the incident.
Typical TMJ symptoms after a car accident include:
-
Clicking or pain in the jaw joint, difficulty chewing or opening the mouth
-
Headaches, migraines, facial pain
-
Ear symptoms: tinnitus, pressure, dizziness
-
Neck and shoulder pain
-
Teeth grinding or noticeable changes in bite
-
Trouble concentrating or sleeping
Why TMJ Disorders Often Go Undiagnosed
TMJ dysfunction is complex and often goes undetected, because:
-
The symptoms are non-specific and can mimic other conditions
-
General practitioners or orthopedic doctors usually don’t check the jaw
-
Complaints appear with a delay and are attributed to stress or unrelated issues
One study found that TMJ dysfunction was significantly more common in patients with a history of whiplash, but had often been overlooked during initial assessments [3].
What to Do if You Suspect TMJ After a Car Accident
-
Keep track of your symptoms – be as specific as possible
-
Mention the accident, even if the jaw pain didn’t start immediately
-
Get a functional TMJ assessment by a qualified dentist or TMJ specialist
-
Inform your insurance provider, especially if the symptoms are accident-related
Treatment Options for Post-Trauma TMJ Dysfunction
An individualized treatment plan can relieve pain and restore jaw function:
-
Functional diagnostic imaging and jaw movement analysis
-
Therapeutic splints (e.g., neuromuscular night guards)
-
Manual therapy or osteopathy
-
Physical therapy and muscle relaxation techniques
-
Stress reduction and nighttime relief
Some studies suggest that early use of TMJ splints after trauma may help prevent chronic dysfunction and reduce inflammation in the joint [4][5].
Conclusion: Don’t Ignore Jaw Pain After an Accident
If you’re experiencing symptoms like headaches, jaw tightness, or ear pressure after a car accident, your jaw joint might be the root cause. TMJ disorders are treatable – the earlier, the better. And remember: Even seemingly minor accidents can have lasting effects on your jaw and posture, especially in patients with deep bite or jaw misalignment.
Do you have questions or suspect TMJ problems after an accident?
Feel free to book an appointment – our practice specializes in TMJ diagnostics and treatment after trauma.
References
-
De Boever, J.A., Nilner, M., Orthlieb, J.D., Steenks, M.H. (2008). “Recommendations concerning definition, terminology and diagnosis of temporomandibular disorders (TMD).” Journal of Oral Rehabilitation, 35(3), 122–132.
-
Lobbezoo, F., Visscher, C.M., Naeije, M. (2006). “The role of occlusion in temporomandibular disorders: an evidence-based approach.” Journal of Dentistry, 34(7), 361–371.
-
Curatolo, M., Bogduk, N., Ivancic, P.C., McLean, S.A. (2011). “The role of the cervical spine in post-traumatic headache and TMD.” The Lancet Neurology, 10(11), 1080–1088.
-
Katzberg, R.W., Westesson, P.L., Tallents, R.H. (1996). “Temporomandibular joint imaging in whiplash-associated disorders.” Dentomaxillofacial Radiology, 25(3), 132–137.
-
Türp, J.C., Schindler, H.J., Hugger, A., Erni, S. (2004). “Management of temporomandibular disorders following whiplash injury.” Schmerz, 18(5), 430–436.
Dr. med. dent. Stefanie Morlok, Zahnärztin und MSc der Kieferorthopädie, Schwerpunkt zahnärztliche Funktionstherapie, Gnathologie, Behandlung von CMD (craniomandibulären Dysfunktionen), www.drmorlok.de, München und Utting am Ammersee. www.cmd-kompetenz.ch, St. Gallen, www.cmd-info.ch